Dr. Rita Charon brings to the examining room a scholar’s love of literature and a radical commitment to listening to patients. A Harvard-trained physician with a PhD in English literature, Charon is the founding Chair and Professor of Medical Humanities and Ethics and Professor of Medicine at the Columbia University Irving Medical Center. As an NEH grantee and the founder of narrative medicine, she has taught health care professionals to look to the humanities for lessons in how to pay more and better attention to what their patients are saying. Here she is interviewed by NEH Chairman Jon Parrish Peede.
Jon Parrish Peede: Rita, it is a delight to be with you for this interview. Welcome.
Rita Charon: I am thrilled to be with you.
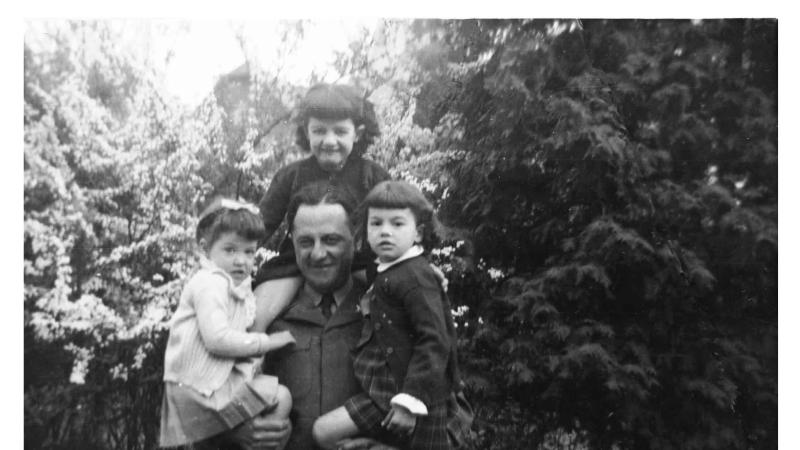
Peede: Your field is medicine. We could also say it is narrative medicine. Or we could say it is the humanities because it is about the human condition. But it starts with family, right? Your father and grandfather were physicians.
Charon: Yes, and it certainly started there. As a girl, I would go to my father’s office. I would sterilize equipment and put the samples away in the back office, though the privacy of my father’s consultation room was sacrosanct. This was in a tiny French-Canadian parish. I knew everybody. My religion teacher would be in there. The parents of the boy I was in love with would be in there. So it was, from the beginning, a very, very intimate business. There was nothing technical or distant about medicine.
Peede: That is my own experience. My father was the town doctor, a surgeon. He had his own x-ray room. So, we would take our little brother and put the x-ray vest on him, which made him topple over. Back then, medicine was a communal act. And now it is something else. Is narrative medicine trying to get us back to basics?
Charon: Narrative medicine is not a parochial act, and it does not require that the physician and the patient belong to the same identity community. What it does require is that the patient and the physician or the nurse or the social worker feel that they are part of a fellowship, but not of belief or race or ethnicity. It is a fellowship of mortality. All of us are going to die. All of us, as humans, live within time, and that is what the humanities can bring to this process of taking care of people as they move toward their end, not to be macabre. I am not macabre. But I think all of us, to the best of our ability, must try to remember that this is temporary. We doctors are not unlike the person in our examining room, the person in the operating room.
Peede: You and I both like the writer Robert Penn Warren. Warren wrote a poem about his mother. He wasn’t, frankly, very close to her. In this poem, he said, “Death is only a technical correction of the market.” Death is, he wrote, “the fulfillment of a wish.” But then he asks, “Whose wish?” And, by implication, he is asking, Whose death?
And that is the piercing, the idea of Whose death? It seems like a natural stepping stone toward the idea of narrative medicine, which is essentially about death.
Charon: Yes. It is about both the universality of death and its particularity. Why does health care need the humanities? Not that it has been devoid of it for all of this time. It is the singularity. You know, my science, my wonderful internal medicine science, teaches me an awful lot about the N of 10,000, these great big samples that are generalizable. And if it is true about this person with prostate cancer, it is going to be true about all of the others.
The humanities not only reminds us, but gives us the science for the N of one. How do I understand so as to do my best for this individual, this eighty-three-year-old woman in my office, who grew up working at Bonwit Teller, the granddaughter of a slave? How do I fulfill my duty toward her, no matter what cacophony of diseases she might have? So that is why we need you.
Peede: You have an MD, and then you went back and got your PhD in literature, writing your dissertation on Henry James. And what James said about literature applies to medicine. He said a great writer doesn’t report but renders. Isn’t this what narrative medicine and your whole career are about?
Charon: Absolutely. When I first read James, I was floored. I was not an English major. I was a bio major. I was on my way to medical school. I pick up an old copy of The Wings of the Dove that somebody had thrown away. I read the novel in three days, and I say, I had no idea anyone could write like this. It was exactly the rendering. It was, How did he know to expand every nanosecond to reveal, to expose what is inside, and to do that for every character and every moment? It floored me. And it is that that brought me to the English department.
I was a doctor, an assistant professor of medicine, and I said, “Can I take a course?”
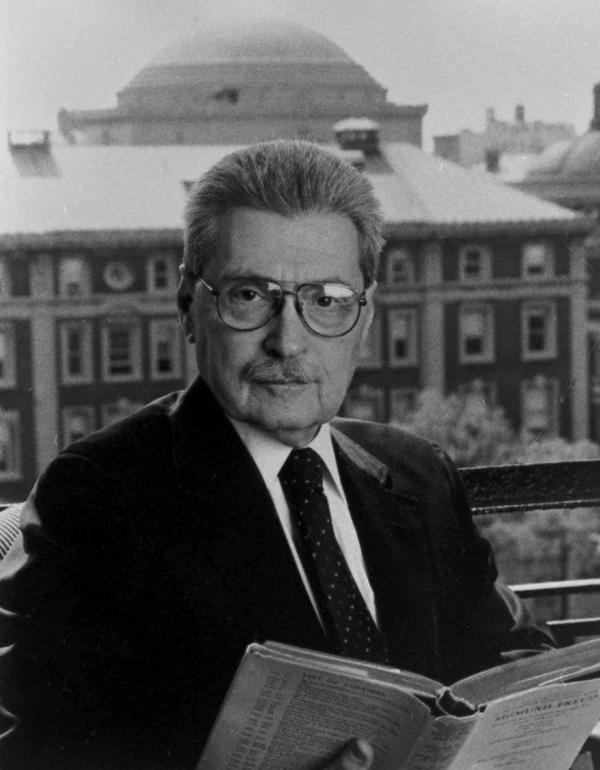
In fact, it was Steven Marcus to whom I said, “Can I take a course?” Steven Marcus was the George Delacorte Professor of English. He studied with Lionel Trilling who, remember, gave the first Jefferson Lecture in 1972. Marcus was the spirit of Trilling, not just at Columbia but elsewhere. It was he, Steven Marcus, who brought the study of literature into the medical school. He did it in the early ’70s, way before I got there. He just died earlier this year, and he was my supervisor. And I miss him so. But it was his spirit that brought the humanities into medical school. And I feel now that this flowering of the work of the humanities in medicine is my tribute back to Steven. And he, wherever he is, is saying, Right on.
Peede: You have published and edited books about narrative medicine. You have received awards, delivered a TED Talk. Now the field is treated as a given.
But what I come back to is that you had an MD from Harvard, yet you went humbly into the English department. And when we think about changes we hope to see in the practice of medicine, I suggest humbleness itself, specifically the idea that there is more learning to be had. Is that not essential?
Charon: Yes. The opposite of humility is what? Arrogance, superiority, maybe even ironic distance? It is the idea that I know more about you than you know. My shoulder goes up. That is the kind of posture that creeps into the physician and the medical student. You have got a mass in the head of the pancreas, a bad thing to have. So I know more about you than you know. I know what that means. Do I not want ironic distance, to be separate from you? Do I not want to be on a plane a little above you?
I can go on about what David Foster Wallace has to say about ironic distance and how what is wrong in the medical setting is, as my students tell me, not a dearth of empathy. It is an excess of irony. That kind of distance, in which I take refuge in the fact that the head of my pancreas is doing just fine. Now multiply that by twenty times a day. So, that accounts for the unavailability, the being out-of-reach that so many people experience with their internist or their surgeon, even their psychiatrist.
Close reading is a way to address that. Reading and entering into other people’s narrative world. It is the imagining, the summoning-up of another narrative world that allows us to . . . I am not going to say understand, but to come near, near to the plight of the person we are trying to help.
Peede: So let’s define narrative medicine. Tell me about the roots of narrative medicine and what it means today.
Charon: For quite a while, my colleagues and I at Columbia called our work “humanities and medicine.” Then I got tired of the ampersand. The phrase “humanities and medicine” didn’t mean very much. I was just finishing up my degree. I had done a lot of work in narrative theory. And so the concepts of narrating, narrative, and story, all of those elements, all of Gérard Genette was very telling to me.
I remember I was writing an article that I was going to submit to the Journal of the American Medical Association. And I didn’t know what to call it. Narrative and medicine, the narrative dimension of medicine, the narrative hemisphere of medicine, it all seemed kind of flaccid. While I am sitting there, this phrase swam into my head, “narrative medicine.” Oh, that is what it is. Why? Because it is a noun. It is a thing you can do and still be a doctor. I practice narrative medicine.
It didn’t take us away from the actual conduct of medicine. And it infused the clinical practice with this other realm of thought that the humanities alone provide, the careful attention to the words and lived experiences of others. So, since 2000, that is what my group and I have called what we do.
Peede: Let’s talk about it at a practical level. So you have a literary text that may be informative and provocative for a health professional or a physician. And they read it. And it serves as an apparatus to help them drill down into what the characters are going through.
Now, I am a patient and I come to see them. With the help of this training, they are going to lean into everything I am going through, what my family is going through, and they are also going to think about how it impacts them as health providers.
If that is not quite it, would you tell us what it is?
Charon: It is along those lines. Steven Marcus would always say, “Every word counts.” And you had to mine the meaning, the implication, the allusion, the beauty out of the language, and pay attention to the figural language, to the temporality, the spatiality, all of those things that we do as readers. And as you get better at it, you do it all at once.
We train people to listen in a way that every word counts and to pay attention to what figures the patients are using. Where do they start? What is the beginning of this story?
And what am I listening as? What is my framework as you are telling me about your visit to the walk-in clinic, because you had a fever and they told you, Oh, by the way, your sugar is up? So, you are a diabetic. So you had better take this pill. Now, a patient told me this not too long ago.
I am not listening only as an internist. I am not listening as a social worker. I am not listening as a psychologist or a psychoanalyst. All of those have frameworks for how to listen. And finally, with great relief, I realize I am listening as a narratologist. I am listening to how the story gets told. At what point do the tears come? At what point does the tempo shift? At what point does the plot change?
By doing that, I stop myself from what some people call binning, putting things into bins, oh, this sounds like acid reflux, oh, this sounds like gallbladder disease. I don’t want to do that.
In a way, it is dumb listening. It is a listening where you don’t know what you are listening for. I am listening for the language, for how it comes out. And then I am able to use the image that the patient has given me. I can say to the young man who is having trouble with his digestion, What you said was your body feels like a metal pipe. I simply repeat what they said. And they’ll say, That’s exactly right!
It is like being a mirror and, yes, humble. And that is how you learn.
Peede: Flannery O’Connor said, “It requires considerable courage at any time, in any country, not to turn away from the storyteller.” Is that part of it?
Charon: Absolutely. God bless Flannery O’Connor because she brought into our lives the savagery—I mean, think of any of her characters—and the grace that goes along with it. So any reader of hers is going to have to face that paradox through and through.
The storyteller is the wiliest, most unpredictable critter. The storyteller is in charge because they are the one who decides what the story is. So if you are listening as a diabetologist, if you are listening as an orthopedic surgeon, you are listening only for a very, very specific subtext.
Many physicians don’t want to hear any of the other stuff, I don’t want to hear about the son in jail. I want to know, Does it hurt more when you pitch the ball or when you catch the ball?
But, typically, sick people don’t come in knowing what is the matter with them. They come in saying, I don’t feel like myself. Where are you going to go with the answer to, Does it feel worse when you pitch the ball or when you catch it? Do you see? It is a matter of radically, radically unframed listening. We are teaching, in our workshops, radical listening, which is a listening unperturbed by what it is I expected to hear. And it is equally powerful in a clinical conversation as it is in a conversation about politics, where nobody agrees. Do you see?
Peede: I would like to know what books, particularly novels or poems, that you come back to.
Charon: Unlike many of my colleagues in this field, I don’t like teaching texts that have illness as their subject or plot. I find it boring and misleading.
Damage has been done to texts. If you teach The Death of Ivan Ilyich to a group of doctors, you know what is going to happen? They argue about, Was it gastric cancer or pancreatic cancer? I am serious. They can’t help it.
So when you teach things too close to a clinical setting, it prevents deep thought. I barely teach William Carlos Williams or Chekhov. What I look for is really thick texts, texts that you can get lost in, hard texts.
I am going to Istanbul in a couple of months for a narrative medicine workshop. And I was trying to think, What are some texts I know that are written in Turkish that I could teach to this group? I pull out Orhan Pamuk’s Snow.
I proposed that we teach the first page of Snow, which is a brilliant, very condensed, opening: The man gets on a bus, but it is told in a kind of posterior past tense. He would-have-been-able-to-had-he-but-known kind of temporality. It is Jamesian in a way. The structure is a form of analeptic prolepsis, a looking forward to look backward. It is luscious. I just taught it a few days ago to a group of pediatricians. And we got lost in the experience of temporality.
Peede: What is fascinating with Pamuk is his whole approach to tense is related to how he develops his narrative. I was talking with him in Mexico for a government project. And he was taking photographs of us as we were having conversations. He photographs his audiences at his panels.
Charon: Really?
Peede: I think that says something about how, as a creative mind, he approaches narrative. I don’t know that a literary scholar could write extensively about his sentences without also writing about him as a photographer or a documenter of his own life.
Your childhood, by the way, sounds to me incantatory. What did you fall in love with? Books, reading? What was the moment?
Charon: As a child, I would get like a dozen books out of the library, climb the apple tree, and just read through them. And they were fairy tales and horse stories and Nancy Drew, early on. I went to college in the ’60s. So we had a war to fight or we had a war to stop. There was a lot of activism in my growing up.
I attended an experimental college. It was called Bensalem. Do you remember Bensalem from Francis Bacon’s New Atlantis? Bensalem was an academic utopia. We read Dante in the original. All students and faculty learned Urdu. We all wanted to start at ground zero and learn together. It was very experimental. It was committed to justice and fairness.
Within narrative medicine, we are committed to social justice, equity, and fairness. We are doing a lot of work now around race and violence and justice because we know that the failings of medicine fall on persons who are not white, who are not middle class, who are not of some means, and they do less well across the board in health outcomes. So, there is a very pointed and all-consuming commitment within narrative medicine to tolerance, justice, and fairness. And that affects what we are going to read. We are trying our very best to not continue a white male canon. We are really widening out what it is that we are learning, teaching, and studying.
Peede: Yet you focused on Henry James. Is it an either/or? You either throw out the canon, or you have a new one, or can we have both?
Charon: You can’t deprive young readers of Shakespeare. You can’t deprive readers of the things that matter. We can hope the work being produced now makes room for the voices that would otherwise be marginalized. But it doesn’t mean that my students don’t read James and don’t read Joyce and don’t read Virginia Woolf. They do, but we need not limit ourselves to that. Reading beyond the old canon challenges us to take in and dig deeply into texts that are very unfamiliar to us. It makes us all students, which is very good.
Peede: We have fewer English majors than we used to. At the graduate level, the topics are more and more esoteric. In the mid twentieth century, through the Book of the Month Club, you would receive books with introductory pieces that were actually very cerebral. But the general public could follow them. Do you think an unintended consequence of narrative medicine is that it may revitalize in some ways literature and literary theory?
Charon: I think it does better than that. I think it brings the humanities into the world. There are some aspects of our academy in the past two or three decades that have removed us from the world, from the now, from the real, from what goes on in the streets among people who are not literary scholars. We have done a lot of such complicated work that we often feel that we are talking to one another. And the others think we are kind of weird.
So many of my colleagues within literary studies feel grateful that it is possible for literary scholars to do something that changes the world, that changes a life, that changes the trajectory of a person, in our case, as they face illness. And it is a deep-moving gratitude: Thank you, Rita, for letting me put my work to use. And it is not like applied. It is not instrumentalizing. I believe it is grasping the capacity of these humanities disciplines and their skills to better comprehend and even contribute to the value of living.
Yes, there are more jobs available to English majors because of medical humanities. I hear from a lot of medical schools looking for junior faculty or even academic departments looking to hire someone in medical humanities. But that is not the only reason. It is really more: that this is an incursion into the material world, the world of—I am going to sound Jamesian—the world of living for the scholar.
Peede: The larger question that our agency, NEH, is dealing with concerns the humanities as a field and an occupation. Parents are looking at tremendous tuition levels and saying, I want my child to be a lawyer, an engineer, a business person. Not an historian or an English major.
Some of the problem is misinformation. We haven’t done the best job of explaining our value. But I am curious to know, What would you say to those parents?
Charon: This is an oblique answer to your question. I get two or three e-mails a week from complete strangers saying, I can’t decide between science and literature, I can’t decide between medicine and a PhD in English, I am writing to you because you seem to be doing them both. How did you do that? How can I?
And my answer is not stock because they are all different, but the answer is, You must do both. It is within our grasp to be highly disciplined, rigorously trained within literary studies, within history, within psychology, within anthropology, within phenomenology or other branches of philosophy, within the fine arts, and have the capacity to put the force and the power to work, be it in diplomacy or psychiatry.
So, granted, it means somebody has to be in training for 15 years, but, you know, we are extending the lifespan. Go ahead.
Now, is that cheating on my part because I want more colleagues? There are only around six or eight MD/PhDs in literature. I want there to be a hundred.
Peede: Could you talk about the difference between the medical humanities and narrative medicine?
Charon: Medical humanities is the category name that includes a variety of specific fields. It includes studies of the history of medicine, literature and medicine, narrative ethics, philosophies of medicine, and qualitative social sciences; whereas, narrative medicine is a more specialized and sharp exploration of the narrativity of the stories of illness and the singular accounts that a person can give of him or herself. It is one aspect of medical humanities. Narrative medicine’s principles derive from literary theory, narrative theory, continental philosophy, and social justice advocacy, while its practice focuses on improving the intersubjective contact of clinical care.
I am very fortunate at Columbia because our College of Physicians and Surgeons attracts many applicants who already have advanced degrees in the humanities. We get persons with MFAs in fiction and poetry. We get musicians who are conservatory-trained. We get persons who have studied maybe not up to the PhD level but certainly the English major, maybe a master’s in a humanities discipline. And they come to us because Columbia has a reputation for encouraging this kind of study. The credits that medical students earn for taking humanities courses on the Arts and Sciences campus count toward their medical degree.
So I have a cohort of humanities-trained medical students, and I can see what they do differently from the others. I can see that it is their humanities training that permits them to perceive that which must be perceived.
I wrote a little piece in Academic Medicine recently called “To See the Suffering.” From rigorous study in the humanities, mostly literary studies and phenomenology or philosophy but the others, too, we learn to perceive and to tolerate the paradoxes that we were talking about before: the savagery and the grace, the sense that one lives forever and the sense that one does not, the awareness that this thing that we consider real, like reality, is an artifact.
Now, you need to go rather deeply into the study of the humanities to really understand the artifice of the real, to understand that your own congress with what is around you is what creates what is around you. I mean, I am just saying ordinary things that any English major knows but not that every medical student knows and perhaps that few doctors know. And, again, that’s what is missing in a transaction where one person is sick and the other person is supposed to be able to look at the savagery. I want every physician to ask himself or herself, What is stalking my patient? And not to ever not know that there is some terror, mystery, or ghost stalking them.
But, instead, do you know what we do? We hire other people to talk to patients when they are dying because we can’t bear to. There is a whole branch of medicine, palliative care, trained in the skills of talking with and caring for people as they near death. Some physicians, not all but some, are grateful that somebody else is going to talk to the patient who is dying.
Peede: Even the vocabulary of how we experience pain can be related to learning. You use words such as grace and savagery, which brings back that same passage from Flannery O’Connor. Quoting St. Cyril of Jerusalem, she says that we all must pass by the dragon on the roadside, which is this idea that sooner or later we are all in mortal danger. Instead of saying to somebody, It hurts, we say anguish. My professor and dear late friend Barry Hannah talked about “unscrolling the hurt.” And I thought that that is what you do as a narrative medicine physician. You are giving somebody the chance to unscroll their hurt. Do we actually teach that in medical schools?
Charon: Well, we are finally starting to, which is a credit to the contribution of writers and literary scholars within the clinical enterprise. The philosopher Nelson Goodman taught us a long time ago that you have to be able to represent what is in front of you before you can perceive it, that you have to confer form in some way in order to perceive something. He says that when we represent what we perceive, we do not copy it. We achieve it. So the achieving of, you see, the achieving is done in the conferring of form.
Our form is captured in language. A photographer will capture in image, a sculptor, et cetera. I am doing more and more work in music and medicine. The composer is capturing form in harmony and disharmony and relative meter and so on. But it is the capturing that allows one to see. And when we are trying to see things that are hard to see, that mass at the head of the pancreas in a patient whom you love already, what do you do? Often it feels that to see it clearly is beyond your capacity.
So that is a roundabout way of saying that the kind of triangulating that is possible in the humanities—I am not looking just at you, I am looking at something that we both can look at—lets us do what needs to be done.
Peede: How do we know it’s working? Or let me put it this way: Is narrative medicine improving patient care?
Charon: We are calling for a science of this work, not anecdote, not, Oh, I had a guy once who . . . , but really credible evidence that there are some differences to be had. There are very few studies. We have done a couple in pediatric oncology and a number of studies among our medical students and clinicians. There are some things we can say with some confidence. We can say with some confidence that rigorous study of literary texts improves the capacity of the clinician to stick with medicine, to avoid the kind of emotional exhaustion that you hear about among physicians that causes them to leave practice and even hurt themselves. Even short bursts of literary work, reading, writing, creative work relieves that emotional exhaustion. And this was found in well-designed trials.
There is a lot of work with patients, but it is spread in many different fields. In the oncology literature, there are some good studies showing that breast cancer patients who have been in ongoing groups where there is creative work—reading, writing, fine arts—live longer than patients equally sick who don’t get that.
Peede: This is arts therapy?
Charon: No, it is not arts therapy. That is kind of different. This is serious work in the humanities and fine arts. It is not toward a psychological clinical goal. It is the work for itself. Art therapists would echo what I just said.
I am the chair of the Department of Medical Humanities and Ethics at Columbia, and I am building a research effort, at least within the Division of Narrative Medicine, that is aimed to show clinical outcomes for this work. Now, that is down the road. When I say, “clinical outcomes,” for example, I may teach the clinicians, the doctors and nurses, something about the care of overweight patients. It is a very big problem because many doctors don’t want to take care of people with obesity.
So we are using narrative methods to break through that kind of bias and to help people understand where it comes from. The outcome has got to be the health of the obese patient. Do you see? So this takes a much longer time, but that’s the goal, to show in metrics that are admissible to the skeptical scientist that this has demonstrable and even predictable effect.
That is going to take some years, but let me tell you it is imminent. It is in the works. That is not a very satisfying answer, but it could only happen on the basis of all that has been done already.
Peede: Your last name is spelled C-H-A-R-O-N. And you had a patient who recognized that name from Greek mythology. Would you tell that story?
Charon: Yes. I was a third-year medical student. I had my red name tag on my little white coat and went into rounds on the first day of my time at this hospital. The patient was twenty-six years old. He had an advanced hepatocellular carcinoma, cancer in his liver. There are six or eight or ten doctors standing around. And the patient looks at my name tag, and he says, “So this is it,” knowing the myth of Charon, who is the ferryman who rows the boat across the River Sytx to Hades and the afterworld.
I was kind of shocked and mortified that I was adding to this man’s suffering and wondering, Where is city hall in Boston? Where do I go to do something about this inappropriate last name for a doctor, even though my father and grandfather had the same name? The young man died two days later.
I didn’t go to city hall, and I didn’t change my name because, as I came to understand it, my mission is to know that journey very well, to know that river. And so from then on, I felt my task was to live up to my name.
Peede: And do you think being a reader and having so much literature embedded in you has helped you ferry people better?
Charon: Absolutely. At the beginning, I was surprised that scenes would come to me as I was sitting with a patient. A literary scene would come to me, and I would say, Why am I thinking about this now?
I was at the funeral of a woman I had taken care of for thirty years. She had lots of diseases. She was very complex, a handful. She had a big and problem-riddled family, a kid who was autistic, and one who was in jail. And while I was at her funeral an image just visited me. The image in The Wings of the Dove when Milly Theale, the young heiress who is about to die, is given her final parting at this palazzo in Venice. And I shook my head, Why am I thinking about Milly now? And it took me a little while to understand that precisely the plight of Milly was the plight of this woman. They had nothing in common except for the drastic nature of the plight they faced, and both women were so brave in facing it. And it was the bravery of my patient that came to me.
But I am sitting there, in the presence of her open coffin. I see her there, this body I had touched and examined for decades. And nobody but Milly could have given me this, the sense of her fortitude and her courage all through her life. Do you see? And that happens routinely.
Peede: Surely some people say to you, What you have in narrative medicine can’t be replicated or scaled. How do you answer them?
Charon: Typically what skeptics say is, Rita, but who has the time to do that? Well, when somebody says, You have eight minutes per patient, the only thing to say back is, Says who? Eight minutes per patient is not medical best practice. It is not. It is a combination, as we know, of bureaucratization, the corporatization, the neoliberal, revenue-first way of life. It is not just in medicine. Ask anybody who runs a department store or works in government.
I think there is a purity about health care that makes us even more willing to speak up, and maybe others are more willing to listen when it is about who is going to die and who is going to suffer.
Those who practice palliative care, who care for persons at the end of their lives, they have been savvy enough to get legislative approval from the people who set the prices for things, that they are allowed to have half-hour interviews, instead of 12-minute interviews. And they will get reimbursed for the full half hour. Do you see? So that is what all of us have to do, is say, No. You know, guys, it doesn’t work this way, no matter what the other interests want. And the interests are legion. It is the hospital executives. It is the insurance companies. It is pharma. It is the device manufacturers. It is those who are making profit on things as they are.
And we have to have the—what do you want to call it?—the muscle, the wherewithal. We have to have the courage and the passion to say, This is not how to practice good medicine. Do you see? So it is a call to arms.
Peede: Well, I want to say what an absolute honor and a pleasure this has been for your insights, your leadership, your inspiration. For the humanities endowment to have you as a guest lecturer, to have you as a grantee, to have you as an adviser, has been a gift to me, my predecessors, to those who come after. And so I want to thank you.