Reba Benschoter readied herself to speak before the crowd of luminaries from industry, academia, and government who had gathered to talk about the transformative potential of new media in medicine. Among those assembled at the New York Academy of Sciences that day in 1966 were a bevy of Manhattan advertising executives, the pioneering Texan heart surgeon Michael DeBakey, the head of the National Library of Medicine, and the governor of American Samoa. As their hosts had explained, electronic media were the source of a biomedical revolution every bit as important as antibiotics, anesthetics, or organ transplants. “Just as seven out of ten prescriptions written today are for items unknown to medicine before World War II,” they concluded, “seven out of ten possibilities for communicating the knowledge behind those prescriptions were not available before 1946.”
Benschoter was there to talk about the most prominent of these communications possibilities: television. Drawing on the thinking of Harold Innis, the Canadian historian of communication, and amplified by his countryman Marshall McLuhan, the academy’s conference retraced the history of media technologies in the practice of medicine. In the argot of McLuhan’s media theory, “hot” media like film and radio engaged one sense entirely and made the viewer or listener into a passive recipient, while “cool” media like television engaged several senses less completely and required more interaction from the user. Television took center stage at the event, partly because of its relative newness, but also because of its interactive potential as a “cool” medium.
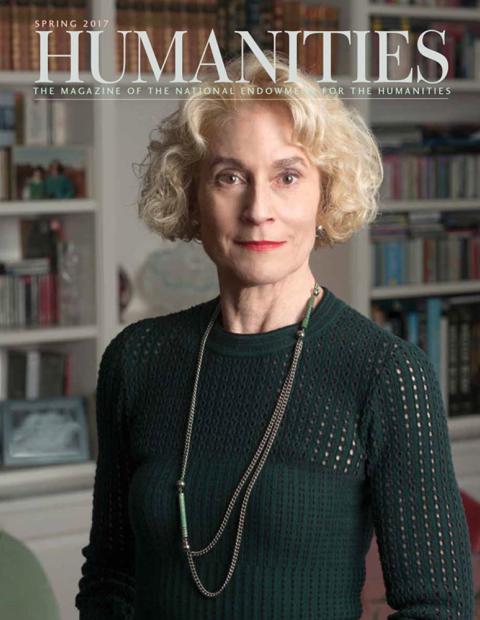
Like many other people in the room, Benschoter worked in communications and studied television as a novel medium for health-science education. But the material she was presenting in New York, based on two years of experience using television at Nebraska Psychiatric Institute (NPI) and the Norfolk state mental hospital, had led her to think critically about the potential for television to create a new infrastructure for patient care. Television, she suggested, was poised to radically change the very nature of clinical medicine, the conduct of biomedical research, and the structure of medical institutions themselves.
The practice of medical care at a distance was not new to the 1960s. As far back as the Middle Ages, many European physicians had received the stories of their patients’ ills in the form of letters—often accompanied by a flask of urine for diagnostic testing—and they offered their prescriptions and prognoses without any face-to-face interaction. Other forms of epistolary medicine continued well into the twentieth century, and continue to flourish in the twenty-first century practice of e-mail medicine.
But the advent of closed-circuit and cable television in the postwar decades precipitated a new wave of attention to the visualizing potential of electronic media. Television was initially known as a broadcast medium that was dominated by the three major networks. By 1966, however, cable TV promised a more interactive network of screens, cameras, and users. As the instantaneity of two-way television opened up different possibilities for virtual presence, medicine became an important spot for imagining the benefits of a newly “wired nation.” Interactive television might make it possible to conduct a physical exam, review an X-ray or a microscopic blood specimen, or even provide psychotherapy in real time for patients situated hundreds of miles from their doctors.
We live today in a world in which each week, seemingly, a new form of new media—from Fitbit to Facebook, electronic medical records to smartphone apps—promises to revolutionize the ways we experience health and illness. But we often forget that our current practices have been shaped by media that were once new. By studying the medical history of television when it was still considered a cutting-edge medical technology, my own research aims to better understand how we conceive and implement new technologies in medicine. What can we learn from what I call the “analog patient” of the twentieth century that might help patients in our digital present? Benschoter’s work and that of her contemporary, Kenneth Bird, who ran an experimental television field station at Boston’s Logan Airport in the late 1960s to the early 1970s, provide some clues.
Reba Benschoter arrived in Omaha in 1957, looking for a job as a psychologist, having recently earned a master’s degree with a thesis on the use of television in education. When she introduced herself to Cecil Wittson, NPI’s head, he urged her instead to pursue her interest in communications media at the newly built Nebraska Psychiatric Institute. Wittson’s experience as a Navy psychiatrist in the Pacific theater had convinced him of the importance of telecommunications in mental health care. After joining the faculty in Omaha in 1950, Wittson began to research using telephones to expand mental health services to rural areas in Nebraska. When NPI was designed in 1955, he had the building wired for closed-circuit television, and hired a technician named Van Lear Johnson to manage the complex network of media technologies.
Within two years, Benschoter, Wittson, and Johnson created a closed-circuit loop between two video cameras, two microphones, and two television sets that connected NPI and the University of Nebraska’s anatomy department across the street. After satisfying themselves that the setup could be used for teaching, they asked a neurologist to conduct a comprehensive patient exam by television, and then asked a psychiatrist to conduct group psychotherapy over the same system. These early proofs of concept—teaching, diagnosis, and therapy—became the basis of a grant from the National Institutes of Health aimed at testing the potential of a longer link between NPI and the state mental hospital in Norfolk, 112 miles away. When the microwave link between the two facilities went live in 1964, the institute initiated the first large-scale test of interactive television as a medical medium.
By the time Benschoter reported these findings at the NYAS conference, the program had been running for more than two years and had clearly established the educational and social value of television in the training of NPI’s resident physicians while they were on their psychiatry rotations at the Norfolk hospital. Psychiatry grand rounds and other events at the University of Nebraska were beamed in from Omaha as “telelectures” so that the residents in Norfolk could listen and occasionally ask questions of their distant professors. It allowed trainees at the satellite institution to feel connected to the main campus. But Benschoter’s work also emphasized how useful television could be for clinical care, patient quality of life, and ward administration.
Because the Norfolk hospital had no staff neurologist, the diagnosis and management of complex neuropsychiatric disorders had previously entailed long delays and depended upon the scheduling of specialists from Omaha, who visited intermittently. Now, however, with a TV screen and camera in front of him, the NPI neurologist could sit down and observe “reasonably detailed” neurological examinations and electroencephalograms (EEGs).
Moreover, the television link connected patients to family members who could not otherwise visit. After Benschoter opened a viewing station at NPI eight hours a week for family members to communicate in real time with their loved ones, these “TV visits” were found to improve the morale of patients, family members, and hospital staff. Before the TV link, only 3 staff psychiatrists were stretched over 27 wards at Norfolk, and the institution was so understaffed that employees often described themselves as custodians rather than therapists. With interactive television, Benschoter and Wittson were able to add regular therapy rounds on each ward staffed by psychiatrists back in Omaha.
This embrace of new media, Benschoter told the crowd at the New York Academy of Sciences, had produced real results for mental health care in Nebraska. “Today,” she concluded “success of the project can be seen in the unlocked doors, the changed staff attitudes, the patient participation in hospital therapy and work programs, and the appearance of the ward itself with its freshly painted furniture and new curtains.” The total inpatient population of the hospital also dropped from more than 900 in 1965 to 476 by the end of 1968. The NPI group took this change as evidence that increased psychiatric services available via television combined with the increased therapeutic use of new drugs and therapies helped return state hospital patients to their families and communities. As Wittson would later claim, the television system had a great symbolic effect. “As one result,” he quipped, “Nebraska may well become the first state to do away with state mental hospitals.”
In later years Benschoter referred to the Nebraska television project as one of the first successful demonstrations in the nascent field of “telemedicine.” On that day in 1966, however, the term had not yet been coined. To understand television’s role in the initial theory and practice of telemedicine, we must turn from Omaha to Boston, from rural care to urban practice and the rather eccentric television field station of a young physician named Kenneth Bird.
On the morning of October 4, 1960, a murmuration of starlings flew into the engine of an Electra turboprop taking off from Boston’s Logan Airport, causing the plane to stall and collapse in the shallow waters of Winthrop Bay. Though many passengers died on impact, a large number survived the crash only to die afterward due to delays in medical attention. As radio broadcasts relayed news of the disaster, hundreds of spectators took to the roads to witness the spectacle, unintentionally blocking the passage of emergency vehicles on key roadways.
Despite being only 2.7 miles away, ambulances from Boston’s Massachusetts General Hospital (MGH) were unable to arrive in time to prevent many needless deaths. In the crash’s aftermath, the director of the Massachusetts Port Authority reached out to MGH head John Knowles to build a “miniature hospital” in Logan to respond to future air emergencies. Kenneth Bird was named the first head of this clinic.
Bird was especially interested in pulmonary and cardiovascular care, and when the Logan Medical Station opened at Gate 23 three years later, he initially conducted studies on disaster management and the impact of airplane noise and jet fumes on hearing and lung function. But the practicalities of running the clinic turned his thoughts toward the role of communications technologies in health care. Bird and his colleague Dr. Joseph Miller staffed the clinic between peak commuting hours of 8 to 10 a.m. and 4 to 6 p.m., and were available by phone to nurses who staffed the clinic 24 hours a day. The limitations of medicine by telephone soon became apparent.
“One of our first patients,” Bird would later recall, “was an elderly woman who had injured her hip. The medical station nurse telephoned me a full report of the woman’s symptoms, but I just couldn’t be sure of the diagnosis: Despite all our efforts I had to face the fact that a verbal report just wasn’t enough in a situation like this. ‘If only I could see the patient,’ I thought. There was no choice but to bring the woman by ambulance to the hospital to determine how extensively she was hurt. But of course I could see patients at a distance. If I could see a space launch a thousand miles away in Florida, and hear an astronaut’s heartbeat a thousand miles up in space, then there was no reason why a patient a few miles away couldn’t be seen and his vital signs checked, while a nurse led him through a physical examination.”
Much as Wittson and Benschoter stretched remote diagnosis from aural to audiovisual by adding television to the psychiatric setting, Bird did the same for the urgent care setting. Though the distance between MGH and Logan was a tiny fraction of the distance between NPI and Norfolk, the task of getting a TV signal between the hospital and airport proved to be more challenging. Privacy concerns had to be addressed, the Federal Communications Commission had to be convinced that the signal wouldn’t be picked up by other sets or interfere with other forms of bandwidth, and Bird, along with engineers from CBS and WGBH, had to figure out how to build it.
With the help of a three-year grant from the U.S. Public Health Service, Bird was eventually able to set up a line-of-sight microwave transmission pathway between the two sites and build his telediagnostic clinic of the future. Closed-circuit TVs were equipped with a range of cameras for long shots and close-ups to aid physical examination; other specialized cameras could transmit X-rays, EKGs, and video microscopy of blood smears. All of this information was fed back to the main hospital to a console of a physician working in an alcove off the emergency department. When the clinic opened in April 1968 to great fanfare, the Boston Globe reported that “the doctors are never more than a few feet away from their patients, even though the latter are at the airport and the doctors are at the hospital downtown.”
A third-year medical student at Harvard Medical School rotating through the clinic described it as one in which “the doctor’s stethoscope is three miles long.” This medical student was Michael Crichton. Just a year earlier his first science-fiction novel, The Andromeda Strain, had been published to critical acclaim and optioned as a blockbuster movie in the emerging genre of the biomedical thriller. He was already at work on Five Patients, which devoted an entire section to describing the science fiction already present in the contemporary practice of the Medical Station at Gate 23.
Like Crichton, Bird often chose to describe his clinic as a form of science fiction in the present. Where Wittson and Benschoter used the television to bring modern metropolitan psychiatry to rural Nebraska, Bird described his jet-setting patient population as denizens of the future. “We always have viewed the 5,000-employee population of the airport as a prototype of one community of the future,” he told one reporter, “heavily dependent upon radio communication, aware of the value of electronic aircraft aids including radar and accustomed to the daily use of closed-circuit television as currently used for flight schedule information. This community already is convinced of the value of applied electronics and thus has set its own stage for acceptance of medical electronics.”
Television was the central technology in Bird’s vision of telemedicine. He is quite likely the first physician to quote the popular media theorist Marshall McLuhan in grant reports, quipping in the 1970 proposal in which he coined the term “telemedicine” that “time has ceased, space has vanished, we now live in a . . . simultaneous happening. Ours is a brand new world of all onceness.” Bird was also fond of McLuhan’s argument that broadcast television, as a form of “cool” media, “permits an intense commitment” and has become “the most recent and spectacular electrical extension of our central nervous system.”
But Bird thought that this cool medium was about to become even cooler, and chided McLuhan for ignoring “the unidirectional limitation of present day television.” Interactive cable television, in contrast, permitted a “dynamic interaction which allows interpersonal communication across distance to recreate, and even enhance, face-to-face communication . . . [w]hen an interactive television system is augmented with medical diagnostic and monitoring instrumentation, a telemedicine circuit emerges.”
The televisual mediation of medicine came with perils as well as promise. In addition to expected fears about privacy, there were concerns about the accuracy of television as a diagnostic tool. Even though color TV was available, Bird and his chief technical collaborator, the CBS engineer Stanley Krainin, preferred black and white. Bird was concerned “that a poor color picture could lead to erroneous patient assessment and diagnosis.” Except in dermatology and some forms of pathology, Bird and Krainin saw color to be largely incidental to medical diagnosis, and focused instead on problems of fidelity of image. Photographs depicting television screens that themselves depicted images of the eye exams of a model patient at two different camera settings were part of Bird and Krainin’s extensive studies of the fidelity of physical diagnosis of patients over the television. If a doctor could see a lesion in the blood vessels of the conjunctiva in person, would that same lesion be visible to another doctor looking at that eye on a TV screen several miles away? The pair steadily tested the influence of different permutations of cameras, lenses, and video-enhancement algorithms on the ability to distinguish key features on microscopic, radiological, and physical examinations.
The telediagnostic clinic encountered some degree of skepticism by patients and practitioners. Bird’s papers at Massachusetts General Hospital contain a piece of doggerel typed on Logan Medical Station letterhead, presumably set to the tune of the 1965 Rolling Stones hit “(I Can’t Get No) Satisfaction”:
I don’t want no Tele-Medicine
I don’t want no Doctor’s smile
Flashing on a television
Over any span of miles
I don’t want no diagnosis
With a 1500 lens
I don’t want no eye exam
With a camera focused in
I don’t want no Doctor peering
Down my throat from miles away
I don’t want nobody listening
To my heart on microwave.
Echoes of Big Brother notwithstanding, Bird’s telemedical field station was widely considered a success—in the words of its nurse practitioners and medical staff, in the accounts of many patients, and in publication after publication about the value of medicine by television.
When John Knowles left Mass General in 1972 to become the head of the Rockefeller Foundation, he took Bird’s concept of television medicine with him as a vision of community medicine of the future. Knowles commissioned a report, An Introduction to Telemedicine: Interactive Television for Delivery of Health Services, which described the Nebraska and Logan television clinics as the first two steps in a new era of telemedical care, one where cable television would provide a technological solution to health-care disparities.
By 1974, the Rockefeller report could point to 11 active demonstration projects that were supported by the National Library of Medicine as well as funders such as the U.S. Public Health Service, the National Science Foundation, and the National Aeronautics and Space Administration. Television medicine was being tested from the inner-city streets of Harlem and the South Side of Chicago to the wilds of northern Alaska, from the Miami-Dade county correctional center to the island territory of Puerto Rico.
All of these programs turned out to be technical successes. And yet like many other Great Society and New Federalist projects funded under the Johnson and Nixon administrations in the 1960s and 1970s, they did not survive the fiscal realities of the Reagan administration. By the early 1980s, all of these federally funded experiments in achieving health-care equity through interactive television closed up shop.
It is worth noting that Benschoter’s optimistic 1966 presentation on medical television of the present had been followed by an equally hopeful pair of medical futurologists. One hospital director noted that the communication of “sensible information” by television could undo the problems of dehumanization and cost increases associated with the overuse of technologies in hospitals. With medical television, he concluded, the hospital itself would soon disappear.
“In the world of tomorrow,” another futurologist suggested, “we will be able to communicate by television as readily as we now communicate by telephone.” By 1990, he predicted, everyone would carry a “picture gun” in their pocket, which would “allow him to readily record images and sounds anytime, anywhere. This masterpiece of miniaturization will be electronic and will carry its own power supply. It will record both still and motion pictures in color, and will be totally self-adjusting for both exposure and focus. . . . Records may possibly be made on small, thin discs of durable material resembling poker chips. . . . This basic tool will also be made in a model which will allow transmission to a specific remote location.”
Although the telemedical demonstration projects of the 1960s and 1970s were discontinued, on some level we can recognize elements of our own present in the future that was being described at the New York Academy of Sciences in 1966. The health benefits of “disruptive technologies” like smartphones, Fitbits, and the Internet of Things are regularly promised to us in popular periodicals and news channels. In Geneva, the World Health Organization’s “mHealth” initiative promises to use mobile digital health technologies to combat diseases such as diabetes, heart disease, chronic obstructive pulmonary disease, and cancer in resource-poor settings. In the United States, the final winners of the Qualcomm Tricorder XPrize, a “$10 million competition to bring health care to the palm of your hand” are expected to be announced as this article goes to press.
As in the 1960s, when concerns about privacy, misdiagnosis, and misuse of information accompanied the adoption of television in medicine, today there are deep wells of anxiety over the health applications of new media. Widespread uptake of electronic medical records, mandated by the Affordable Care Act, has revolutionized medical notation practices over the past decade. Although these records offer greater integration between outpatient and inpatient care, many patients complain that physicians now spend more time in the examination room looking at the computer than looking at them. In my adopted hometown of Baltimore, a hospital system was effectively paralyzed in 2016 after its servers were hacked and held for ransom unless the company paid a fee in Bitcoin to regain access to key patient data.
The smartphones, wearable devices, and data architectures of the present day form a technological substrate that poses social, cultural, and economic possibilities that are different from those posed by cable television in the 1950s, 1960s, and 1970s. But like digital medicine in the early twenty-first century, television medicine in the late twentieth century linked new electronic media to promises of health equity and low-cost, high-value health care. As Michael Crichton noted in his observation of Bird’s television clinic in Logan Airport, North American medicine has been living with promises of science fiction for decades, if not centuries.
Excavating these past visions of the future—and examining the hopes and fears surrounding older technologies when they were first developed—offers the chance to help distinguish which of the promises of today’s new medical media are likely to turn from science fiction into science reality—and which of them are likely to remain in the realm of fantasy.